May 2, 2014 at 3:00 PM ET
OPERATOR: Welcome and thank you all
for holding. I would like to remind all parties that your lines are on
a listen-only mode until the question and answered segment of today’s
conference. This call is being recorded. If you have any objections,
please disconnect at this time. I will now turn it over to Tom
Skinner for opening remarks.
TOM SKINNER: Thank
you all for joining us as we discuss the first case of Middle East
Respiratory Syndrome Coronavirus infection (MERS) in the United States.
Today we have with us, Anne Schuchat, who is the director of the
National Center for Immunization and Respiratory Diseases here at CDC.
She will provide some opening remarks and then when we get to your
questions; she's going to be joined by Ms. Pamela Pontones, who is the
state epidemiologist for the Indiana State Department of Health. Now I
would like to turn the call over to Dr. Anne Schuchat.
ANNE SCHUCHAT:
Thank you, Tom and thank you everyone for joining us today. I want to
provide you with some information on a rapidly evolving situation. The
first confirmed imported case of Middle East Respiratory Syndrome
Coronavirus, known as MERS-CoV, has been reported in the United States.
The patient, a healthcare provider, recently travelled from Saudi
Arabia where outbreaks of MERS are occurring. The patient is currently
in a hospital in Indiana. The patient is isolated, in stable
condition, and being well-cared for. The Indiana public health
laboratory tested specimens from the person using MERS-CoV testing kits
developed by CDC, and today CDC confirmed the test results in our
laboratory. CDC is working closely with the Indiana state health
department and hospital to rapidly respond to and investigate this
situation to help prevent the spread of the virus.
MERS-CoV is a virus that is relatively new to humans
and was first reported in Saudi Arabia in 2012. Most people who have
been confirmed to have MERS-CoV infection developed severe acute
respiratory illness, with fever, cough, and shortness of breath. As of
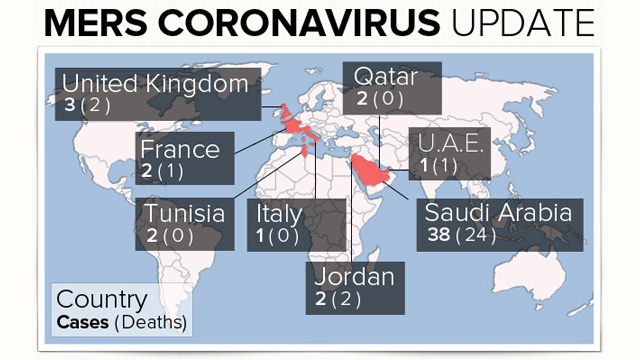
today, including this importation into the U.S. 252 people in 12
countries have been confirmed to have MERS-CoV infection; 93 of these
people have died. Based on the information we have so far, people
with pre-existing health conditions (comorbidities) or weakened immune
systems may be more likely to become infected with, or have a severe
case of, MERS-CoV.
So far, all MERS cases have been linked to six countries in or near the Arabian Peninsula.
Since March 2014, there has been an increase in the
number of cases reported from Saudi Arabia and United Arab Emirates.
The reason for this increase in cases is not yet known and public
health investigations are ongoing.
There is no available vaccine or specific treatment
recommended for MERS-CoV. We do not know where the virus came from or
exactly how it spreads. In some countries, the virus has spread from
infected people to others through close contact. However, there is
currently no evidence of sustained spread of MERS-CoV in community
settings. The virus has spread in hospitals though; the largest
reported outbreak to date occurred April through May 2013 in eastern
Saudi Arabia and involved 23 confirmed cases in four healthcare
facilities.
CDC has been working with partners to better
understand the risks of this virus, including the source, how it
spreads and how infections might be prevented. In this interconnected
world we live in, we expected MERS Co-V to make it to the United
States. We enhanced surveillance and laboratory testing capacity in
states to detect cases, we developed guidance and tools for health
departments, we provided recommendations for healthcare inspection
control and other measures to prevent disease spread. We provided
guidance for flight crews, ems units and customs and border protection
officers about reporting ill travelers to CDC. We disseminate up to
date information to the public, international travelers and our public
health partners. Let me share some more information with you about
the first MERS patient in the United States and what we are doing now
in collaboration with the hospital and state public officials to
respond. On April 24 the patient traveled by plane from Saudi Arabia
to London, England and from London to Chicago, Illinois. The patient
took a bus from Chicago to Indiana. On the 27 of April, the patient
began to experience respiratory symptoms including shortness of breath,
coughing and fever. He went to the hospital on April 28 and admitted
on that same day. The patient is being well cared for and is
isolated. He is currently in stable condition. Because of the
patient’s symptoms and travel history, Indiana public health officials
tested for MERS-CoV. The Indiana state public health laboratory and CDC
confirmed MERS-CoV infection in the patient this afternoon.
The lab and CDC have both confirmed MERS Co-V
infection. CDC and the state health department do not yet know how the
patient became infected, how many people have had close contact with
the patient and whether they have become ill. We do know that many
healthcare providers and workers in the hospitals have varying levels
of contact with the patient. Indiana hospital is using full
precaution. Standard contact and airborne to avoid exposure within the
hospital and among healthcare personnel and other people interacting
with the patient as is recommended by the CDC. As part of the
prevention and control measures, officials are reaching out to provide
guidance about monitoring their health. The first U.S. importation
represents a very low risk to the broader general public. Then in some
countries, there has been limited spread of the virus from person to
person through close contact such as caring for or living with an
infected person. However, the virus has not shown the ability to
spread easily from person to person in community setting. It is very
concerning that the virus has spread in hospitals and we should not be
surprised if additional cases are identified among the healthcare
providers who had close contact with this patient before the patient was
isolated and special precautions were implemented.
People will understandably be concerned by this news
and want to know what they should do. CDC advises that people help
protect themselves by washing hands often, avoiding close contact with
people who are sick, avoiding touching your eyes, nose, and mouth with
unwashed hands and disinfecting frequently touched surfaces. We don't
know exactly how this virus spreads but we encourage people to take
these common steps. At this time, CDC does not recommend that anyone
change travel plans. People who develop a fever or cough or shortness
of breath within 14 days after traveling from countries in or near the
Arabian Peninsula should see a healthcare professional and mention their
recent travel. While sick they should stay home from work or school
to reduce spreading illness to others. Others who should monitor their
symptoms include those who have close contact with someone who has a
fever and cough or shortness of breath after the other person has
recently traveled to another country in or near the Arabian Peninsula.
Those are the two groups that need to take special attention about
their symptoms.
Healthcare providers should be aware of -- after 14
days of traveling from countries in or near the Arabian Peninsula.
They should contact their state or local health department and collect
appropriate specimens. We have great guidance on our website. The
introduction of MERS Co-V is another reminder that diseases are just a
right of way. MERS is now in our heartland. Strong public health
symptoms to rapidly respond and detect are critical to finding and
preventing unnecessary spread of disease. This situation is very
fluid. We expect to learn much more in the coming days. Our guidance
and recommendations may change as the situation evolves. We will share
updated information through additional press conferences and through
the CDC and Indiana department of health website. Now I would like to
turn things back over to Tom and answer the questions that you may
have.
TOM SKINNER: I think we're ready for questions, please.
OPERATOR: Certainly. At this time
to ask a question on the phone lines, please depress star one and
record your name when prompted. Star one, please. Our first question
today comes from Miriam Falco. Your line is open. Please state your
affiliation.
MIRIAM FALCO: I’m from CNN medical
news. Thanks for taking the questions. You said the patient was in
stable condition. What does that really mean? And how infectious was
this patient on the plane? On the bus, and in the hospital?
ANNE SCHUCHAT: Let
me begin with the answer, the patient is requiring oxygen support at
this time and the patient is generally stable. The patient isn't
requiring a ventilator for respiratory support. The patient is getting
excellent care in Indiana. In terms of the airplane, it's very
important to say that at this time in this investigation, we are
approaching this with an abundance of caution. And so that assuring
that we notify contacts through the conveyances that the patient was on
and those close contacts in the healthcare facility or family is
really being taken out of an abundance of caution. We have no
information at this time about spread in any of those settings but we
want to make sure and alert people about the potential risk. As a
reminder, this virus has been exported from the Arabian Peninsula to
other countries. In those settings, there was limited if any spread
but the spread that happened did include others in the healthcare
settings or in the family in terms of the airplane and so forth, we're
out of an abundance of caution want to assure that we're following up
with those contacts. Next question Please.
OPERATOR: Our next question comes from Mike Stobbe.
MIKE STOBBE: Hi,
it's Mike from the Associated Press. Thanks for taking my question.
You said that the patient is a healthcare provider. Could you be more
specific? A physician? Could you say that the gender and the age and
did that person have a pre-existing condition? You mentioned
pre-existing condition.
ANNE SCHUCHAT: Sure, Mike. Thanks
for that question. As you can imagine, protecting the information of
an individual in an investigation like this is very important. What I
can tell you is that the patient is a healthcare provider who was
providing healthcare while in Saudi Arabia. The additional details
we're really trying to protect the individual and that person's
family. Next question, please?
OPERATOR: Our next question comes from Jane Baranowski.
JANE BARANOWSKI: This is Jane from
NBC. I’m wondering if you are releasing the name of the airline or bus
line this person was on to warn other passengers?
ANNE SCHUCHAT: Thank you for that
question. Sometimes we do need to put a very broad alert out. We are
working closely with the department of homeland security and the
airline industry so that we can direct the focus in a more targeted way
to the people who actually were on the airline. So we don't
anticipate needing to do a broad alert about airlines at this point but
have had very good collaboration with the industry right now. We
prefer that because it can focus the greatest attention on the people
who do need to be contacted. As you know sometimes we do need to go a
bit wider. So we are not releasing that information at this time.
I think our next question and I want to clarify, I
have been told if people have a follow up question, they're allowed
to? I guess if you have a follow up, you have probably already
disconnected.
JANE BARANOWSKI: I do, what is the incubation period before the symptoms start to show?
ANNE SCHUCHAT: We
think about five days between infection and when you start to be
symptomatic. We have that 14 day period after travel. There are some
people; there are just a few people that have that longer tail. So
again out of an abundance of caution, we have got that 14 day period in
with the travel history. But most of the patients that have clear cut
exposure to someone else have become ill within five days. Thank you
for that question. Next question?
OPERATOR: One moment, please. Once
again, if parties would please press star one to ask a question. Star
one to ask a question. Our next question comes from Michael
Caldwell.
MICHAEL CALDWELL: This is Michael
Caldwell, ABC News. I wonder if there is any plans to do background
surveillance for the workers in the hospital? The case fatality rate
here seems very high but I recall when West Nile Virus started we
thought the case fatality rate was high and we eventually learned it
was not as bad as we thought. I’m wondering where we are with that.
ANNE SCHUCHAT: Thank you. Some of
the reports coming out of the investigation in the region suggest that
there are some asymptomatic patients. Some people have been followed up
as contacts in the Middle East and are found to be without symptoms
but have a positive test. There is a very active investigation in the
facility and working closely with the Indiana health department and
the details are still being worked out. When there is a new infection
like this about which little is known, it can be very important to
learn as much as possible quickly so that we can improve our guidance
and our protocols. So I think that this particular situation is one
where we really hope to be able to refine the guidance that we give
based on additional information gained in the first several days.
That's a chance for me to remind people that today we may have certain
guidance and in the future it may change as we learn more and we
realize that we can be a little bit more relaxed or need to be a little
more strict. But at this point, we do know there have been people
identified in other countries who have the virus identified through the
chain reaction test who did not have any symptoms. That case fatality
rate of about a third or 30 percent or so is based on the symptomatic
patients. So there is a lot more to learn about this virus that is
relatively new. Did you have a follow up?
MICHAEL CALDWELL: No, but it does give me some sense that the case fatality rate may be a lot less than we're noting right now.
ANNE SCHUCHAT: I think that is
possible. But I do want to say that for respiratory viruses that have
symptoms this is a very severe clinical presentation. To have about a
third of people with any symptoms dying, of course we look over time.
We have been tracking that new virus and the fatality ratio may change
but we have been looking at this particular virus since 2012. As I
think I mentioned we're seeing the clinical illness in people who are
older with underlying medical conditions and we're seeing about a third
of them die from the virus. It's a very serious virus. We hope to
learn much more but we want to take this very seriously and not assume
that it's a mild issue. But again, things can change. That's what we
know now based on about two years of people investigating this in
several countries. Next question?
OPERATOR: Our next question comes from Rob Stein.
ROB STEIN: It's Rob Stein from
National Public Radio. Thanks for taking my call. Can you tell us
where in Indiana this patient is and anything more about any of the --
anybody else on the plane or the bus or anybody else that this person
has come in contact with shown any symptoms yet?
ANNE SCHUCHAT: Let
me begin by saying we are trying to allow the investigation to go
forward and the facility to respond locally. We aren't aware now of
anyone else with confirmed illness. We have a very active
investigation on. I think I would say it’s way too early for us to
breathe a sigh of relief that no one else is ill and we will be
actively investigating in the groups that I mentioned. I think that the
doctor may want to say more but in general we would really like to
keep this at the high level rather than on the facility. Next
question?
ROB STEIN: I’m sorry. Can I follow up?
ANNE SCHUCHAT: Yes, I’m sorry.
ROB STEIN: You're saying that you're
not saying anything about where in Indiana this patient is? And are
you saying that you some other folks might have gotten infected?
ANNE SCHUCHAT: No, no. Let me be
very clear. We do not have reports of any other patients ill with the
MERS coronavirus in this investigation. But it’s a very active
investigation and very early. We only confirmed the virus this afternoon
and we are just beginning to look at others. But this is not a
telebriefing based on a cluster if illness in the United States. This
is a single patient who has imported the virus and is ill here. We are
trying to protect the specifics of the location so that is why I am
not mentioning that here. That is pretty standard protocol for this
kind of thing. But to say that we will update regularly and if there
are additional cases, that is the type of reason that we would make
updates. At this point, people are working very actively to try to
understand whether others are ill and they are alerting people to look
for signs and symptoms and they are also letting the clinical community
know what they need to do in terms of evaluating those patients and
making sure that people who do develop symptoms are isolated and not
able to spread further. We don't have any confirmed illness of the
MERS coronavirus beyond a single case that I am describing at this
point. So, sorry if I wasn't clear about that. Next question?
OPERATOR: One moment, please. Our next comes from Betsy McKay. Your line is open and please state your affiliation.
BETSY MCKAY: Hi,
it's Betsy McKay from the Wall Street Journal. Dr. Schuchat, I
apologize, I’m talking from a cell phone so if the reception is
terrible, I apologize. I missed some of what you said earlier. So if
I could just ask you to clarify, did you say the person who is a
healthcare provider was given healthcare in Saudi Arabia or actually
providing healthcare in Saudi Arabia? Is this your assumption or do
you have knowledge that this patient probably got infected in a hospital
or healthcare setting in Saudi Arabia? That's where they got
infected?
ANNE SCHUCHAT:
Thank you. The person was providing healthcare in Saudi Arabia and was
not ill in Saudi Arabia. The person developed symptoms in the United
States. The assumption is the person acquired the illness in Saudi
Arabia. We can't confirm that it is from the hospital or the
healthcare facility and that would be part of an active investigation.
We know there is quite a bit of disease in Saudi Arabia right now that
is under investigation. Next question, please?
BETSY MCKAY: Can I ask one quick follow up.
ANNE SCHUCHAT: Sorry. Sure. Go ahead.
OPERATOR: I’m sorry. We lost her connection.
ANNE SCHUCHAT:
Okay, all right. Let's keep going. I know we have a number of others.
Hopefully everyone's questions will get answered through someone
else. Next question?
OPERATOR: Amy Birnbaum, CBS News, your line is open.
AMY BIRNBAUM: I’m
sorry. I missed her question. I just wanted to follow up and ask was
that healthcare worker working particularly with MERS, helping out in
any sense with patients who had MERS, given that I know there has been
healthcare workers who have gone over specifically to investigate that
outbreak. Thank you.
ANNE SCHUCHAT: We don't have that information at this time.
AMY BIRNBAUM: Thank you.
ANNE SCHUCHAT: Next question?
OPERATOR: Next question comes from Lena Sun, Washington Post. Your line is open.
LENA SUN: Hi.
Thanks for taking the question. Can you clarify how far along are you,
are folks in contacting the people who were on the plane and the bus
and I assume the hospital where this patient is? It would be easier
to, you know, to check. But where are we in that process?
ANNE SCHUCHAT: We're very early in
that process. This is an active investigation. We really just got the
laboratory confirmation this afternoon. And you know, at CDC and in
public health in general we're committed to tell you what we know when
we know it. So that is actively happening right now and we will update
as we learn more from the investigation.
LENA SUN: So can I just follow up,
then? Does that mean you were waiting to get the laboratory
confirmation from CDC before you had the airline reach out to the people
on the plane to say, okay, you know, how close were you sitting to
this person in the seat? Or has that already been started?
ANNE SCHUCHAT: Let me clarify, there
are many things that have been happening simultaneously. And this is
very active. So we didn't wait until we contacted every single person
before we alerted the media and the general public. We have initiated
many things in the past day.
LENA SUN: The other follow up question that I had is do you know whether this person was in contact with any camels?
ANNE SCHUCHAT: That's a great question and I don't
know the answer to it. I don't believe we have an animal exposure
confirmed at this point but thank you for the question. Next question,
please?
OPERATOR: Beth Galvin, your line is now open and please state your affiliation.
BETH GALVIN: Hi, I’m with Fox 5
Atlanta. Thank you very much for talking to us on this short notice
today. I want to, if you could, a little bit talk about the MERS
virus, how contagious it is and just what level alert is the CDC on
with this case here in the U.S.?
ANNE SCHUCHAT: The MERS virus is of
great concern because of the virulence. We have seen clinical
respiratory illness that can be fatal up to a third of the time. On
the other hand it has not yet shown the ability to be easily spread or
transmitted in the community. We are not aware yet of confirmed
community transmission. In healthcare facilities with good infection
control practices, we don't expect substantial transmission of this
virus. And our focus, though, is in the healthcare context before it's
recognized that a person may have this illness, whether there was
unprotected exposure to it. So we don't have a sense right now that
this is very easy to spread but out of an abundance of caution we are
really focusing in on the healthcare contacts and the close contacts
because we don't want to take any chances. Next question?
OPERATOR: One moment. Our next question comes from Caleb Hellerman. Your line is open and please state your affiliation.
CALEB HELLERMAN: Hi it’s Caleb
Hellerman, CNN. Thanks for taking the question. One thing, you have
been talking about matters of days. I wonder if you could expand a
little bit more on the time line of when this person was in The Kingdom
and when they might have come back and was it in April or any more you
can say to pin that down?
ANNE SCHUCHAT: The person traveled
on April 24th from Saudi Arabia to London and then on to Chicago,
Illinois. And so, they were in The Kingdom before the 24th. I don't
have the details of how long but I believe it was, you know, a
substantial period. And so they have been in the United States since
April 27th, and were admitted to a hospital on the 28th of April. So
it's relatively soon since this person returned to the United States
and we're closely looking at the contacts since they have returned
here. Of course in these situations, we're in close contact with our
international partners who are doing other parts of this
investigation. And of course, many countries are investigating suspect
MERS as they have been since the virus emerged in 2012. Did you have
a follow up?
CALEB HELLERMAN: A quick follow up.
You talked about sort of the level of how contagious or transmissible
this might be. Could you be more specific about what constitutes the
kind of precautions in a healthcare setting that you think would make
you not worried about transmission and maybe those weren’t being taken
where she was?
ANNE SCHUCHAT: No, no. We think that the care was very good where the patient has been—
CALEB HELLERMAN: Or where she got infected.
ANN SCHUCHAT: The number of steps
that can happen in a healthcare facility depend on what type of
transmission you expect. There is something called contact and droplet
and airborne transmission. And basically for the general public,
people may need to wear masks around a patient. You may want to put
them in a room where the airflow is protected and doesn’t spread.
There is physical barriers that you can set up. Certainly we do
standard precautions for everyone in terms of hand washing and
protection around bodily fluids. This is a fairly medically technical
set of issues but I would just say that we have no reason to think that
there was inadequate care for this patient and that at this point with
the suspicion and now confirmation, extreme measures are being taken
to make sure there is no exposure that is unprotected to this patient.
Next question?
CALEB HELLERMAN: Thank you.
OPERATOR: Bob Roos, your line is open. Please state your affiliation.
BOB ROOS: I’m with CIDRAP News.
Thanks for taking my question. Can you say anything about where in
Saudi Arabia the person was working? I know Riyadh was mentioned. Was
the patient working in Delta by any chance?
ANNE SCHUCHAT: The information that
we have is that the patient was working in Riyadh and that's where they
flew out of. Did you have a follow up?
BOB ROOS: No. Earlier someone
asked what kind of healthcare provider the person was and I guess you
can't say any more about that correct?
ANNE SCHUCHAT: That's right. Just that the person was working in a healthcare facility.
BOB ROOS: All right. Thank you.
ANNE SCHUCHAT: Sure, next question.
OPERATOR: Molly McCray you line is open and please state your affiliation.
MOLLY MCCRAY: I’m with KPIX out of
San Francisco. I’m just wondering. You say the first case of MERS was
reported in 2012 and you’ve an increase in March of 2014. Are you guys
actively tracking if this virus is mutating at all? Is the CDC
involved in that? Do you have any ideas why you have this surge in
2014?
ANNE SCHUCHAT: Thank you for that
excellent question. There has been an increase in cases since March of
this year. We actually did have more cases in the spring of last year
as well. So there's some question of whether the factors that lead to
MERS may have a seasonal pattern. But of course another question
that emerged with these last several weeks of cases whether there's
been a change in the virus to make it more easily transmissible. There
is one isolate of the virus that was collected recently from a patient
in Saudi Arabia that was sequenced and reported and there had not been,
according to that report, changes in the virus that suggested any kind
of mutation. So based on the sequence of one viral isolate recently,
we haven't seen changes. We will continue to monitor the situation. As
you know with viral outbreaks, that's something that is very important
to keep a look out on. With the SARS virus 10 years ago, 11 years ago,
we do believe there was a change in the virus that led to more
explosive transmission. We will continue to look at that but we don't
have data to confirm that has happened.
MOLLY MCCRAY: May I have a follow
up? I just wanted to find out how you working with your, you know,
other entities, I guess in the Arabian peninsula in tracking this and
taking a look at what is going on with the virus. Who are you guys
working with? Is it just the CDC doing this?
ANNE SCHUCHAT: Not at all. The
World Health Organization has really pulled together the different
countries. We have both international partnerships that are
multilateral such as through the World Health Organization and
bilateral as well. So the CDC has done some investigations in the
region. Other countries have done their own investigations or invited
experts from other places. So this is, you know, in 2014, these new
diseases are just a plane ride away, it's really important that we
cooperate internationally and that's been absolutely vital with the
MERS response. That's a lesson that we have been learning over and
over as we really try to strengthen global health security worldwide. We
need every country to be strong and we need to work together
effectively and we're doing that right now. Did you have a follow
up?
OPERATOR: We can go on to Allison Wyckoff your line is open and please state your affiliation.
ALLISON WYCKOFF: Hi this is Allison
Wyckoff with AAP News with the American Academy of Pediatrics. And Dr.
Schuchat, are there any cautions specific to children that you would
like to emphasize that could be helpful to pediatricians or parent?
ANNE SCHUCHAT: We really have
general precautions rather than specific to young children. I know
that young children often have fever and respiratory symptoms. But the
key here is, is there a history of travel within the past 14 days to
the Arabian peninsula or contact with someone? And then they should
alert their clinician about the travel or contact. The other thing to
say is while the age range in this illness so far is very vast. I
think the youngest reported case was two years old, but the median age
of the case is around 60 years of age. There have been some young
people, some children, some others, but the cases tend to be
middle-aged or I believe it's 51, not 61. So 51 is the median age. So
it's middle-aged people on average but there have been very young and
much more elderly folks. I would just say for pediatricians, all of
those kids with the high fever and respiratory symptoms, ask a travel
history. The emerging respiratory viruses really need a travel history
to raise suspicion. Um, next question, I think we have time for two
more questions.
OPERATOR: Next we have Emily Gertz, you line is open and please state your affiliation.
EMILY GERTZ: Hi,
I’m Emily Gertz with Popular Science. Doctor, can you describe what
the treatment is generally and if it's any different the treatment
being provided for this woman in the states?
ANNE SCHUCHAT: The treatment for
MERS coronavirus is a non-specific. That means that we treat the fever,
we treat the breathing difficulties with extra oxygen but there is no
specific medicine like an anti-viral drug that targets the
MERS coronavirus. And so that is what is being done here and what’s’
being done around the world. We know that some people are doing some
research into particular anti-viral drugs but there is no recommended
specific treatment at this point other than the supportive or
non-specific care. So I think we have time for the last question,
Laurel?
OPERATOR: Certainly, our final question comes from Kyle Thomas. Your line is open, please state your affiliation.
KYLE THOMAS: Hi,
this is WTHR, the NBC station in Indianapolis. I know you can't give a
specific facility but I’m wondering if you can give us a city or region
of Indiana where this patient is located.
ANNE SCHUCHAT: Thank you for that
repeated question. I can tell you that the patient's hospitalized in
Indiana. We do need clinicians around the country not just in Indiana
to be on the alert in terms of travel associated severe respiratory
illness. We think an active investigation in Indiana is going to help
us understand what, if any risk there is, beyond the individual
patient. I really want to thank everybody for participating in the
conference call. We have been talking about how interconnected the
world is and how new diseases can be just a plane ride away. The first
U.S. importation of MERS coronavirus represents a very low risk to the
general public. Public health authorities in Indiana and surrounding
areas are doing an active investigation to make sure we can control
this condition. We will update as additional information occurs. I do
want to remind people that at CDC's website, CDC.gov and at the
Indiana health department website, we will be posting a lot more
information and trying to keep that updated. We will hold additional
press conferences if important changes occur. Thank you so much for
participating. Tom?
TOM SKINNER: Thank
you everyone, and thank you Laurel, for participating. Those who have
follow up questions or need additional information can call the CDC
press office at 404-639-3286. This concludes our call. Thank you very
much.










No comments:
Post a Comment